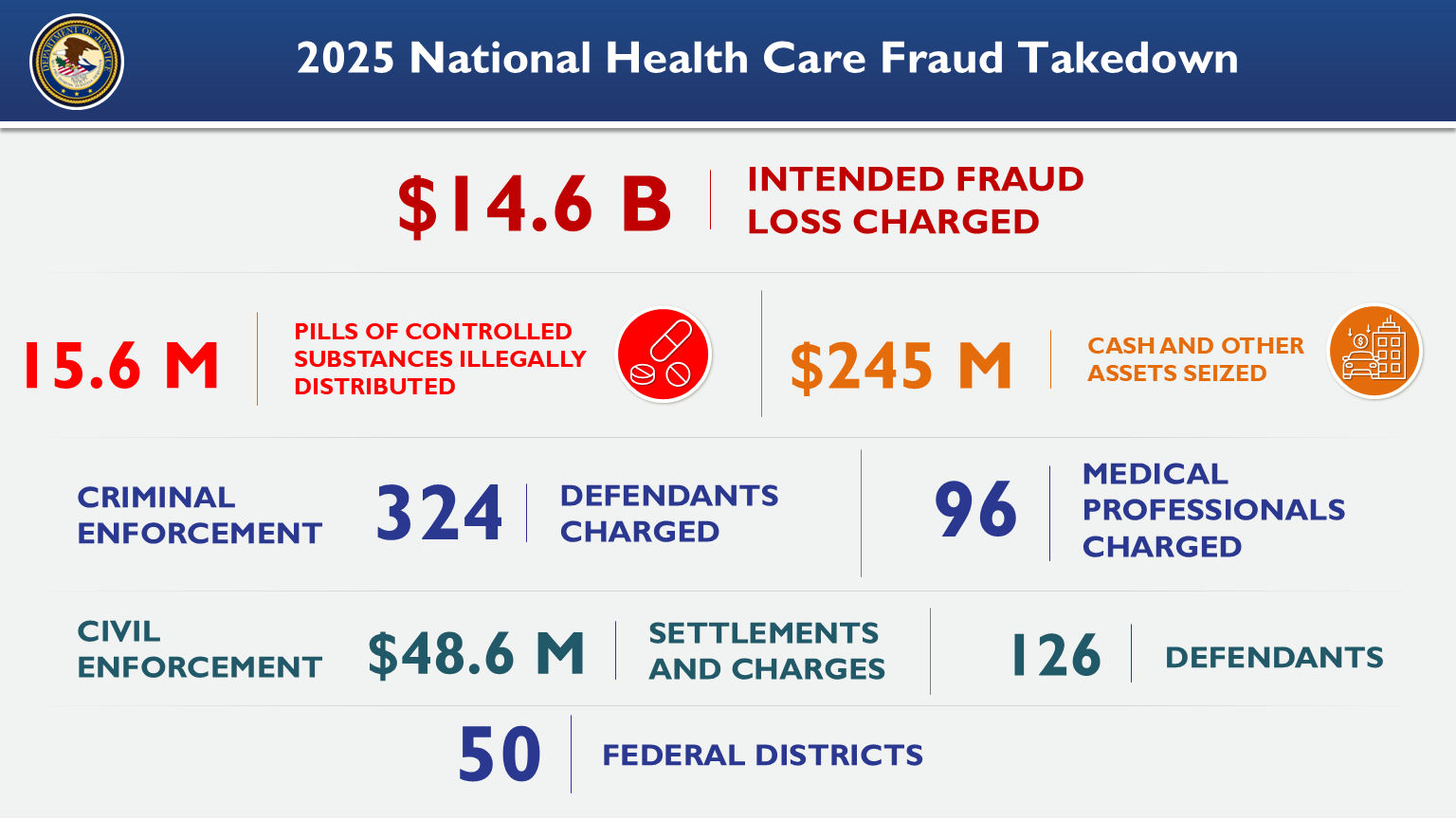
Fraud in the healthcare industry is a significant issue, siphoning billions of dollars away from essential medical services and programs. Recently, law enforcement agencies executed one of the largest healthcare fraud takedowns in history, charging 324 defendants in connection with over $14.6 billion in alleged fraudulent activities. This crackdown is a bold step forward in the fight against healthcare fraud, and its broader implications serve as a stark warning to wrongdoers and a rallying call for all stakeholders in the system to remain vigilant.
A Historic Takedown
Healthcare fraud takedowns aren’t new, but the scale of this operation shows just how serious the problem has become. Coordinated efforts by federal, state, and local authorities uncovered staggering schemes that exploited government programs like Medicare and Medicaid, private insurance companies, and unsuspecting patients.
To put things into perspective, $14.6 billion is enough to fund thousands of hospitals, supply medications for millions of patients, or cover years of crucial healthcare research. Instead, these funds were funneled into the hands of individuals and organizations gaming the system. The charges against the 324 defendants highlight the types of abuses that pervade the industry—and the serious consequences of getting caught.
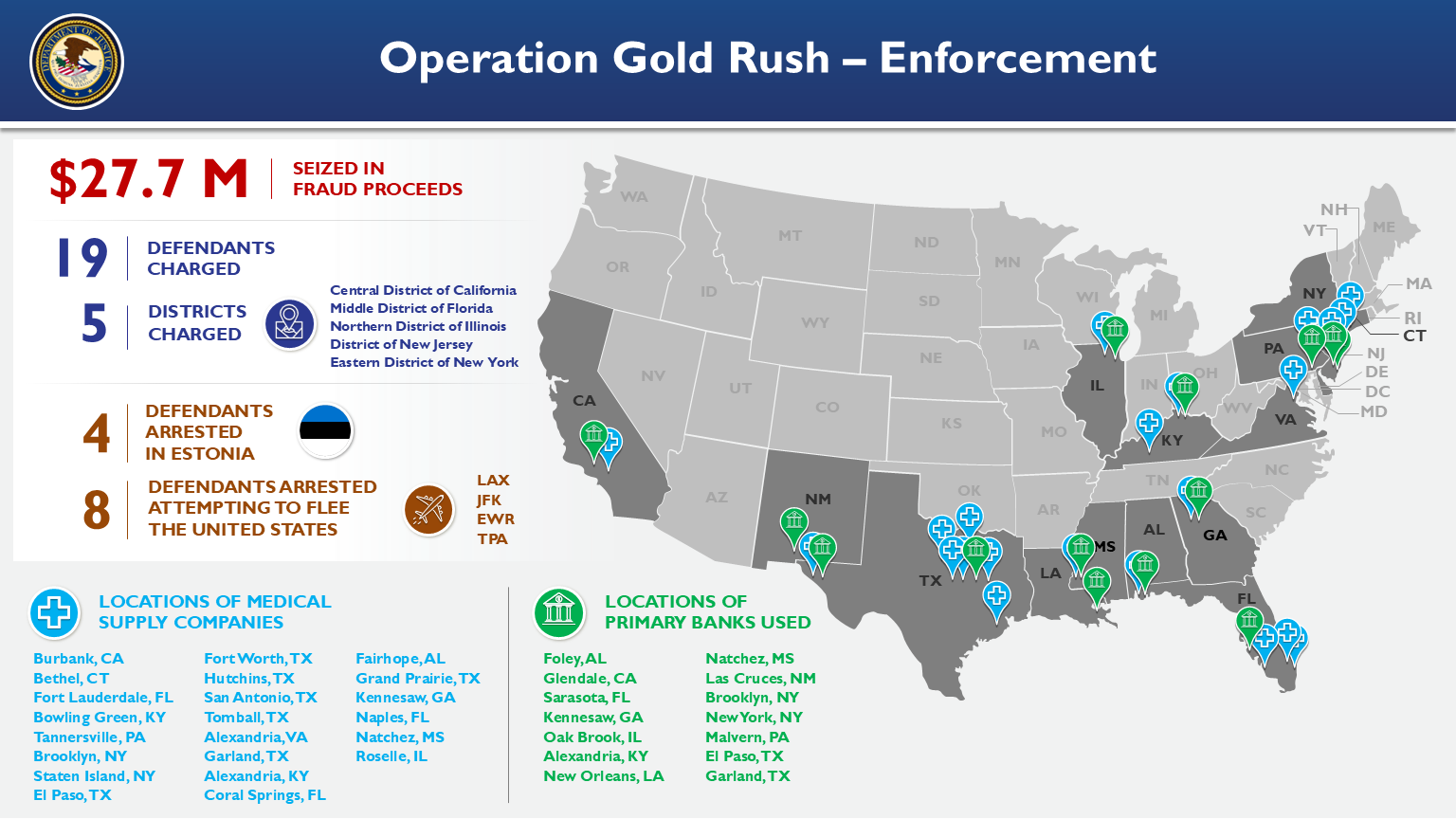
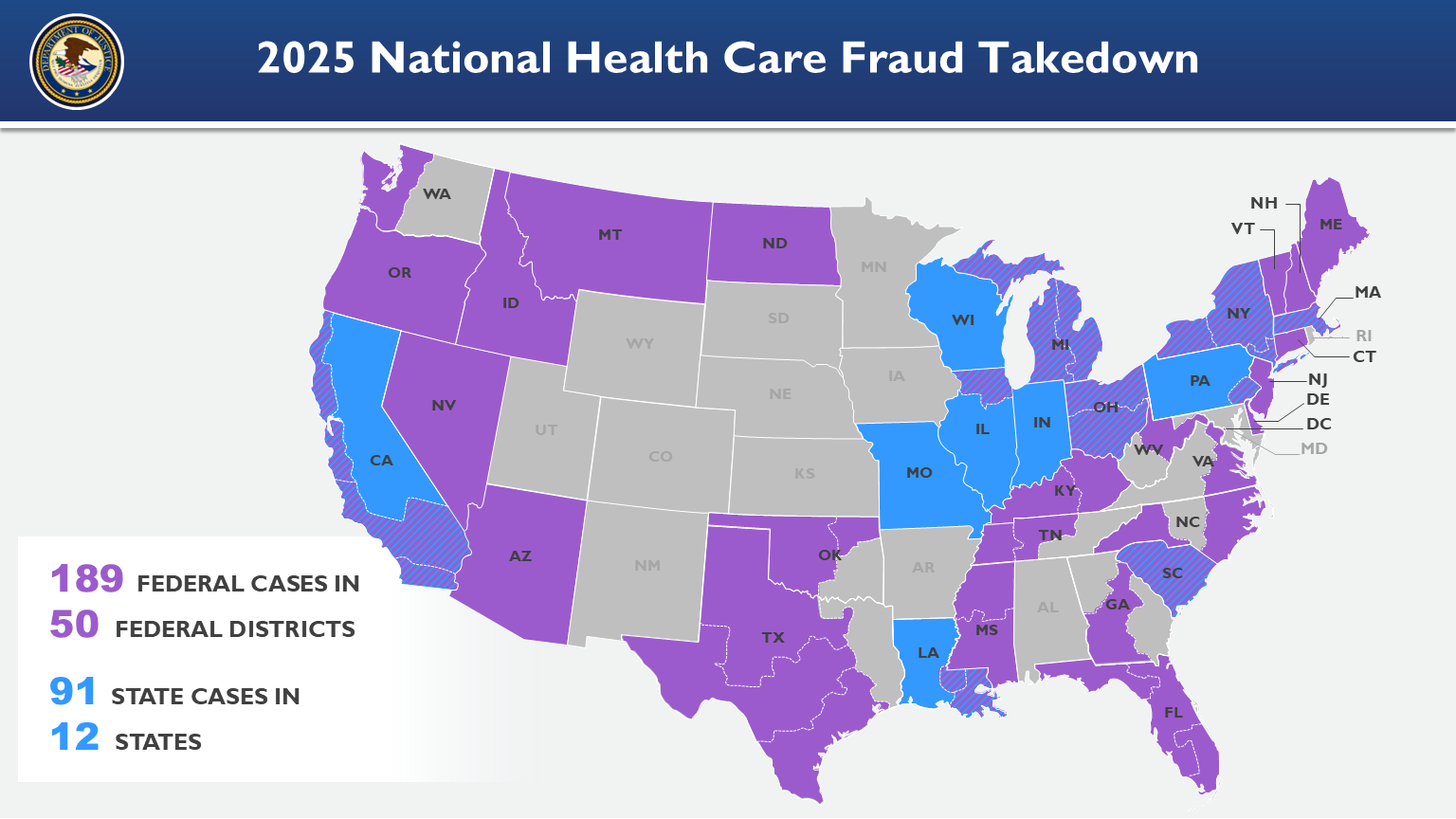
This nationwide takedown exemplifies what law enforcement agencies can achieve when working collaboratively. The Department of Justice (DOJ), the Department of Health and Human Services Office of the Inspector General (HHS-OIG), and the Federal Bureau of Investigation (FBI) were among the primary organizations involved in this intensive operation.
Fraudulent Activities Uncovered
The schemes exposed in this takedown were as varied as they were audacious. Below are some of the most common types of fraudulent activities identified:
1. False Claims and Billing
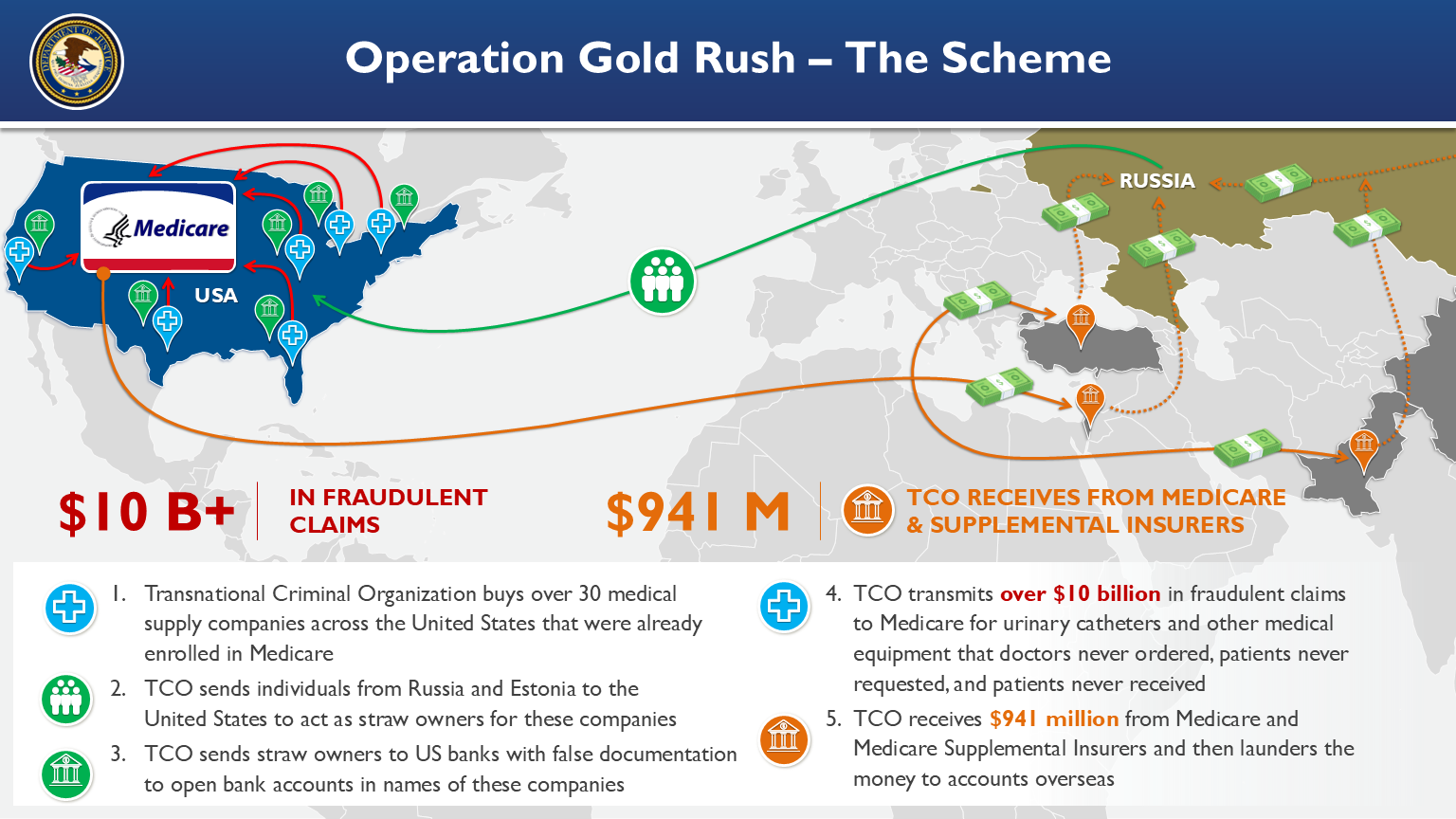
Many defendants were found guilty of submitting false claims to Medicare, Medicaid, or private insurers. These false claims often involved billing for services that were never provided, inflating the cost of services, or billing for unnecessary medical procedures. For example:
-
- Some healthcare providers billed Medicare for expensive tests or treatments that patients never underwent.
- Fraudsters exploited common medical practices like lab tests or drug prescriptions by inflating the volume or exaggerating their necessity.
2. Kickbacks and Bribes
Kickbacks were also a prevalent component of these schemes. These involve unlawful payments or bribes to doctors and healthcare providers in exchange for patient referrals or prescriptions of certain medications. Such kickbacks create incentives to prioritize profit over patient wellbeing.
3. Telemedicine Fraud
With telemedicine on the rise, fraudsters found new avenues to exploit virtual healthcare services. They submitted fraudulent claims for virtual consultations that never occurred or for telemedicine services that weren’t medically necessary. The rapid expansion of telehealth services during the COVID-19 pandemic provided new vulnerabilities for criminals to exploit.
4. Opioid-Related Schemes
The opioid crisis remains a pressing national issue, and this takedown revealed several schemes related to the abuse of prescription opioids. Criminal operations were found falsifying prescriptions or illegally distributing opioids, often for financial gain rather than medical necessity. Such activities not only defraud insurance systems but also contribute to the devastating consequences of the opioid epidemic.
Impact on the Healthcare System
The cost of healthcare fraud extends well beyond the billions of dollars lost. The ripple effects touch patients, providers, insurers, and taxpayers alike.
1. Strained Healthcare Resources
Financial losses mean fewer resources are available for legitimate healthcare services. Fraud drains funding that could improve patient care, enhance medical facilities, and support vital healthcare programs.
2. Increased Costs for Patients
Fraudulent activities drive up the overall cost of healthcare. When insurance companies lose money to fraud, those costs are often passed along to patients in the form of higher premiums or copayments.
3. Erosion of Trust
Fraud undermines trust in the healthcare system. Patients depend on providers and insurers for life-saving care, but when fraudsters exploit this trust, it damages the credibility of the entire system.
4. Public Health Risks
Certain fraudulent schemes, like the overprescription or illegal distribution of opioids, have direct consequences for public health. Fraud also encourages unnecessary medical procedures, which can harm patients rather than help them.
Law Enforcement’s Role in Fighting Healthcare Fraud
This massive takedown is only one step in a long battle against healthcare fraud. The success of this operation was made possible by the unwavering efforts of law enforcement agencies and essential partnerships across industries. Here’s how such initiatives are helping combat fraud:
1. Advanced Data Analytics
Modern healthcare fraud investigations employ sophisticated data analytics tools that detect fraudulent patterns in billing and claims data. These technologies allow investigators to identify anomalies that might signal fraud.
2. Interagency Collaboration
The scope of healthcare fraud necessitates partnerships across agencies. For example, the collaboration between the DOJ, HHS-OIG, and FBI in this operation highlights the power of combined resources and shared intelligence.
3. Public and Private Partnerships
Law enforcement is not alone in tackling fraud. Partnerships with private insurance companies help create a united front against fraudulent activities. Insurers provide data and insights that complement government efforts.
4. Holding Defendants Accountable
Charging and prosecuting individuals and organizations involved in fraud sends a clear message: such crimes will not go unpunished. By seeking penalties and restitution, authorities aim to recover lost funds and deter future fraud.
The Path Forward
While this takedown represents a major victory, more work lies ahead to protect the healthcare system. Patients, providers, insurers, and regulators all have roles to play in ensuring integrity within the industry. Here are a few actionable steps:
- Strengthen Reporting Mechanisms: Patients and healthcare workers should be encouraged to report suspicious activities without fear of retaliation.
- Increase Awareness: Education campaigns can help the public recognize signs of fraud and understand the importance of vigilance.
- Enhance Oversight: Regulators must continue to refine fraud detection systems, particularly as new technologies like telemedicine expand opportunities for exploitation.
Final Thoughts
The National Health Care Fraud Takedown is a landmark event in the fight against fraud, underscoring the seriousness of these crimes and the high stakes of protecting healthcare resources. With 324 individuals charged and $14.6 billion in damages uncovered, the operation is a stark reminder of the importance of vigilance, accountability, and collaboration in strengthening our healthcare system.
The path to eradicating fraud may be long, but with continued dedication from law enforcement, policymakers, industry leaders, and the public, the integrity of the system can be safeguarded. By rooting out fraud and holding perpetrators accountable, we ensure that healthcare remains accessible, affordable, and fair for everyone.